Melanoma skin cancer (black skin cancer) is the most dangerous type of skin cancer and one of the most dangerous types of cancer in general, as it can metastasize even in a symptom-free stage and at a small tumor size. For patients in the late metastasis stage, i.e. with tumors in other organs, the 5-year survival rates are less than ten percent and current therapeutic approaches cannot achieve a real cure. In early tumor stages, however, the chances of recovery after complete removal (excision) of the melanoma are very good. The staging of suspected malignant melanoma during the clinical diagnosis determines how much healthy tissue needs to be removed during the surgical intervention to respect safety margin requirements. Melanoma can current only be diagnosed with the help of tissue biopsies. The tumor thickness or depth of invasion is a key criterion for the tumor staging and is crucial for further treatment and prognosis. In general, the primary development goals of melanoma diagnosis and treatment are the improvement of tumor detection including a reliable preoperative tumor thickness assessment combined with the avoidance of unnecessary interventions.
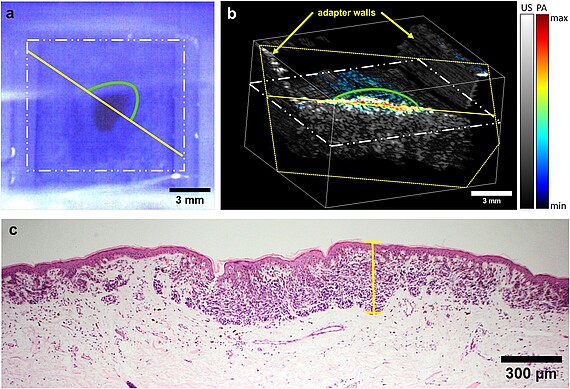
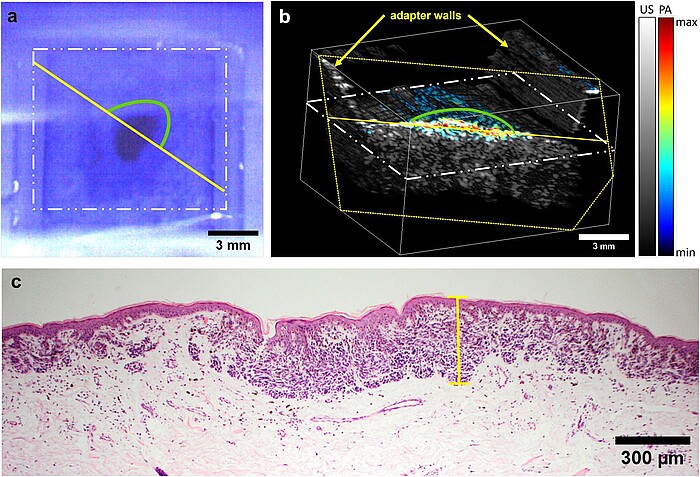
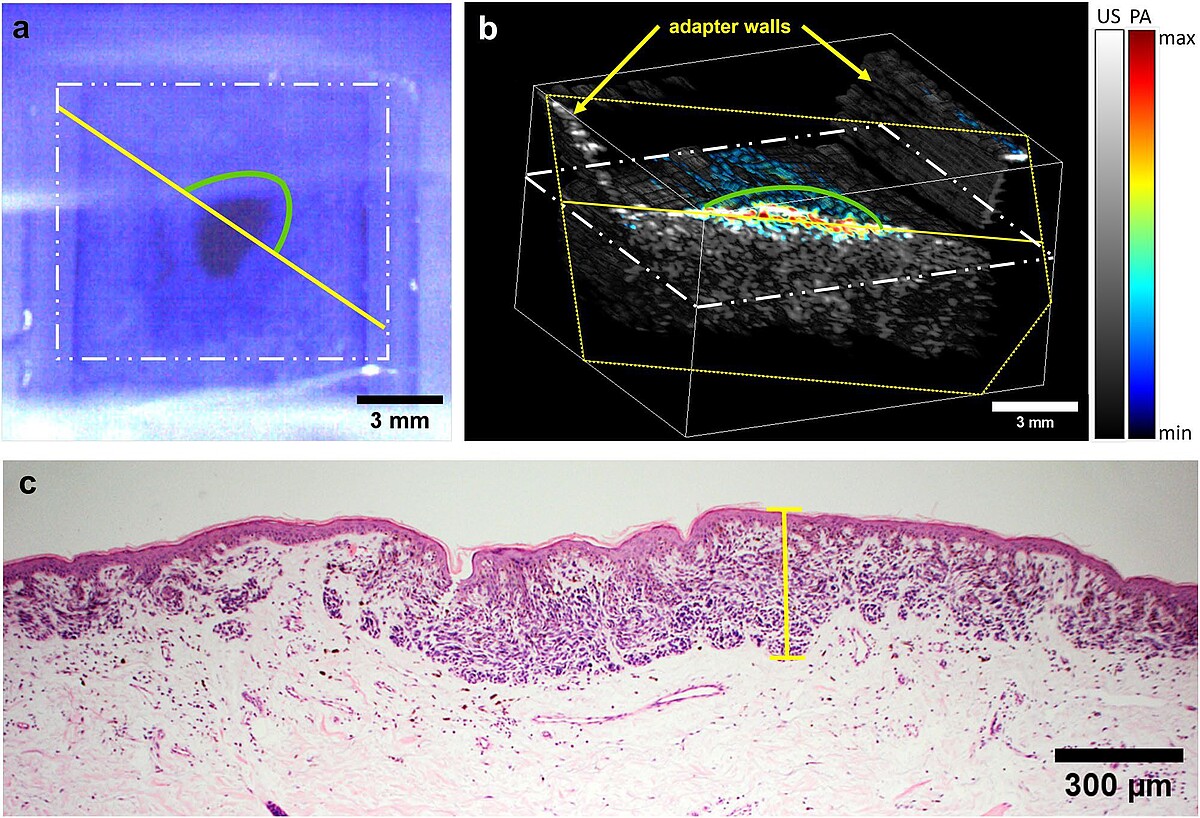
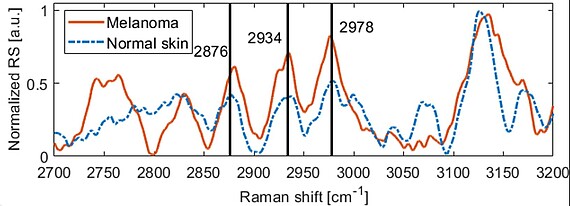
In this project, a method for the preoperative determination of the thickness of skin lesions suspected of melanoma is developed and validated, see Fig. 1 for the current version. Since individual methods have not yet offered a satisfactory solution, a combination of different optical methods is necessary. The imaging system currently developed enables doctors for the first time to reliably determine tumor thickness preoperatively with a high level of accuracy in order to minimize the removal of healthy tissue. In addition, the system is intended to provide spectroscopic and morphological information that allows a more precise determination of the tumor stage preoperatively, in particular whether the tumor is limited to the top layer of the skin, the epidermis. The reliable and precise thickness determination of tumors with thickness up to several millimeters is currently not possible preoperatively and, together with the additional pathophysiological information, would represent a significant improvement in dermatology. The new system meets this need and enables in vivo measurements below maximum permissible exposure levels, see Figs. 2 and 3. To increase sensitivity and specificity, a database is built from the clinical measurements and artificial intelligence (AI) algorithms are used to carry out the classification to improve skin lesions.



References
-
Non-invasive 3D imaging of human melanocytic lesions by combined ultrasound and photoacoustic tomography: a pilot study, AF Kukk, F Scheling, R Panzer, S Emmert, B Roth, Scientific Reports 14 (1), 2768 (2024)
-
Non-invasive optical biopsy of skin lesions by multimodal system with OCT, ultrasound, photoacoustics and Raman spectroscopy, AF Kukk, D Wu, R Panzer, S Emmert, B Roth, Proc. Photonics West 2024 (San Francisco, USA), Multimodal Biomedical Imaging XIX 12834, 56-61 (2024)
-
Combined ultrasound and photoacoustic C-mode imaging system for skin lesion assessment, AF Kukk, F Scheling, R Panzer, S Emmert, B Roth, Scientific Reports 13 (1), 17947 (2023)
-
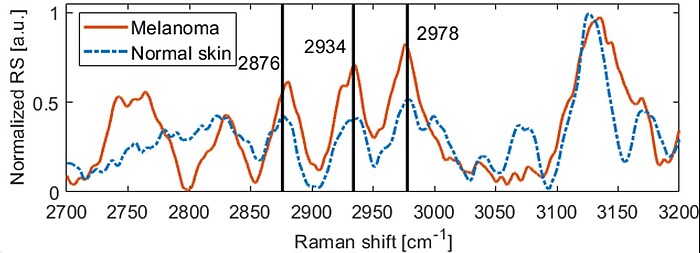
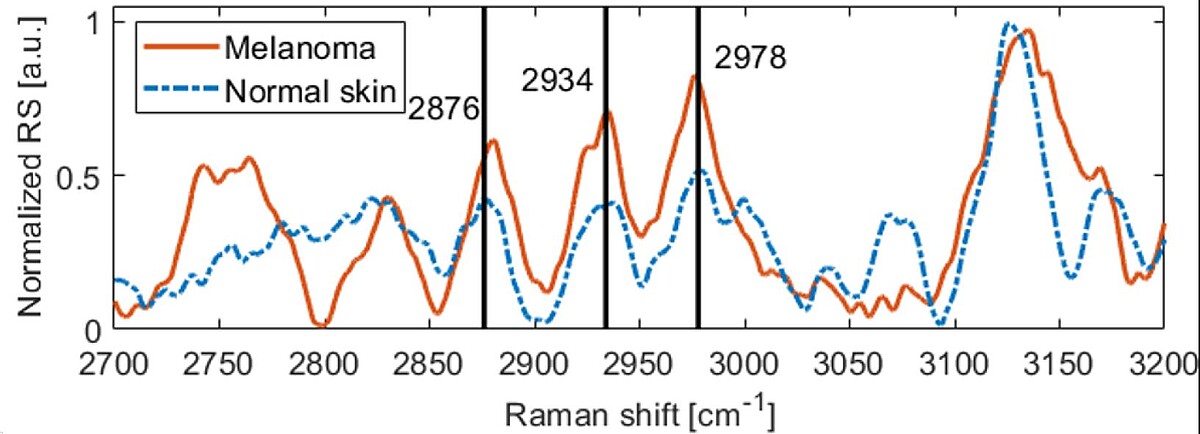
Detection of melanin influence on skin samples based on Raman spectroscopy and optical coherence tomography dual‐modal approach, D Wu, AF Kukk, B Roth, Journal of Biophotonics 16 (8), e202300080 (2023)
-
Multimodal system for optical biopsy of melanoma with integrated ultrasound, optical coherence tomography and Raman spectroscopy, A Fedorov Kukk, D Wu, E Gaffal, R Panzer, S Emmert, B Roth, Journal of Biophotonics 15 (10), e202200129 (2022)
Research Projects
-
Multimodal system for the optical biopsy of melanoma skin cancerThe focus is on the development of a novel system for the optical biopsy of skin cancer. The approach uses a combination of four mostly optical modalities to determine the parameters relevant for diagnosis as well as artificial intelligence for the rapid classification of skin lesions. It therefore contributes to the digital transformation in healthcare and is also suitable for telemedicine applications.Led by: Prof. Dr. Bernhard RothTeam:Year: 2020
-
Non-contact dermatoscope for detection and examination of suspicious skin lesionsThe standard method for the examination of skin lesions is contact dermoscopy. With the contemporary contact-type dermoscopes, lesions have to be scanned manually by imaging each lesion in direct contact with the skin. Although established this procedure has several drawbacks as it is time consuming, has poor reproducibility, and may even be painful for the patient. A non-contact remote dermoscope can overcome these drawbacks and furthermore allow automatized screening protocols. Thus, this project revolves about the development of a non-contact dermoscope for detection and examination of suspicious skin lesions.Led by: B. Roth, M. Wollweber, U. MorgnerTeam:Year: 2017
![]()
![]()
-
Determination of melanoma thickness via optoacoustics and optical coherence tomography (OCT)Development of a method for the preoperative determination of the thickness of melanoma suspicious skin lesions.Led by: B. Roth, M. Wollweber, U. Morgner, M. RahlvesYear: 2013Funding: BMBF
![]()
![]()
-
Skin cancer screeningDevelopment of a digital dermoscopy device with extended diagnostic scope for automated whole-body skin cancer screening (early detection of melanoma)Led by: M. WollweberYear: 2012




